Exploring Delivery Methods and Enhancing Bioavailability in Medical Cannabis Prescribing
Interview with Dr. Joel Wren
Read time: 5-6 mins
Dr Joel Wren unpacks emerging technologies, delivery formats, and clinical considerations shaping cannabinoid therapy in Australia.
Bioavailability is more than a pharmacokinetic curiosity, it's central to clinical efficacy. Dr Joel Wren, a GP and experienced cannabis prescriber, recently joined Adam Isaac Miller for an in-depth conversation exploring how novel delivery methods are enhancing bioavailability and how increased bioavailability and genetic factors shape medical cannabis prescriptions.
Technologies to Increase Cannabinoid Bioavailability
Enhancing the bioavailability of cannabinoids is an ongoing focus in cannabinoid medicine research, especially given that traditional oral formulations often yield low and inconsistent absorption, typically ranging from 6% to 20%. However, Technologies such as Vesizorb™, nanoemulsions, liposomal encapsulation, cyclodextrin-based complexes, and self-emulsifying drug delivery systems (SEDDS) represent promising advancements. Through different mechanisms, these delivery systems are overcoming the inherent lipophilicity of cannabinoids, improving solubility and bypassing first-pass hepatic metabolism.
While exciting, Dr Wren notes, “prescribers are not always told the full story. A lot of it’s protected IP.” This opacity makes clinical decision-making more complex, often relying on limited human data or logic extrapolated from preclinical models.
For instance, high-fat meals can improve absorption due to enzyme release (lipases), but more advanced adjuncts may significantly change dosing thresholds.
Clinical Implications and Dosing Adjustments
These improvements in absorption are more than fun pharmacokinetic factoids, they carry real-world implications for dosing thresholds, side effect profiles, and drug interactions, particularly for medications metabolised via cytochrome P450 enzymes.
Dr Wren recounts that a product representative suggested that a 25 mg Vesizorb™ CBD capsule might equal the bioavailability of 100 mg of conventional CBD oil. If substantiated by independent data, such claims have major implications for dosing, drug interactions and potential side effects.
As cannabinoid formulations become more bioavailable, prescribers must consider lower therapeutic windows, particularly in vulnerable populations or those on concurrent medications such as warfarin or cancer treatments.
“The foundation of bioavailability is the formulation in the first place, right? Are we talking about an oral oil? Inhaled product? PR per rectum?” Dr Wren explains that delivery format plays a pivotal role in patient compliance and response to cannabis medicines.
Individual patient needs, ranging from sensory sensitivities to hepatic or gastrointestinal considerations, demand flexible and innovative cannabinoid delivery strategies. While oral oils remain common, they present variability in absorption, delayed onset, and palatability issues. Inhalation methods, though currently widespread in the Australian cannabis space, come with drawbacks such as short duration of action, inconsistent dosing, and regulatory or social stigma.
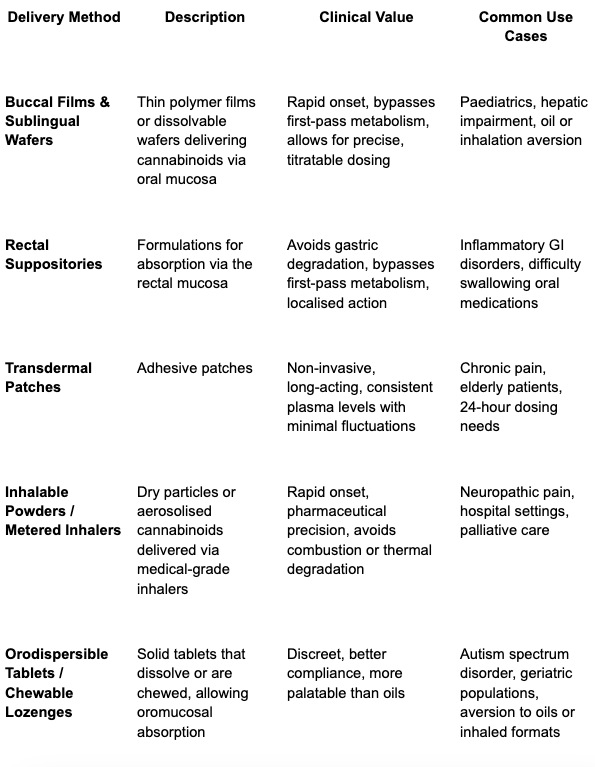
As a result, research is turning to novel delivery systems seeking a balance of pharmacological precision with patient-centred practicality. The table below summarises several methods gaining traction in therapeutic contexts.
Case Examples: Cannabis Wafers and Compounded Options
Individual patient needs, ranging from sensory sensitivities to hepatic or gastrointestinal considerations, demand flexible and innovative cannabinoid delivery strategies. While oral oils remain common, they present variability in absorption, delayed onset, and palatability issues. Inhalation methods, though currently widespread in the Australian cannabis space, come with drawbacks such as short duration of action, inconsistent dosing, and regulatory or social stigma.
“I have one patient with autoimmune hepatitis,” shares Dr Wren. “So her liver is fairly damaged. She's kind of keeping in a bay at a low-dose of prednisone, a steroid that she's taking indefinitely. We experimented with oils for a little bit, and it just wrecked her. So we swapped over to a sublingual wafer.” For this patient, by side-stepping first-pass metabolism in the liver, side effects from the cannabis disappeared, and her desired symptom control was achieved.
The delivery method and formulation also affect patient compliance and, therefore, therapeutic outcomes. For example, in paediatrics or for people with autism spectrum disorder (ASD), oil-based formulations are often poorly tolerated due to taste and texture.
Wren highlights how compounding pharmacies can be instrumental in tailoring formulations. “I also work quite closely with local compounding pharmacists to see what they can do. And one in Adelaide, he makes a powder. I think it's acacia with some guar gum or some sort of emulsifier”. This powdered format allowed one Level 3 ASD patient to take his medication sprinkled on toast, vastly improving administration consistency.
Capsules with gelatin or acacia-based powders also allow caregivers to disguise dosages in yoghurt or custard, enhancing palatability and compliance.
Prime Examples of Personalised Cannabinoid Medicine
One of the most nuanced areas in cannabinoid prescription is balancing isolate vs. full-spectrum formulations. While full-spectrum products may offer enhanced entourage effects, isolates can be useful in cases where specific symptoms fluctuate day-to-day, allowing patients to tailor their intake in real time. For instance, a patient may choose to forego a daytime full-spectrum CBD or THC medication on a low-anxiety or low-pain day, while still utilising an isolated CBN compound in the evening to support sleep.
“I've got one patient in particular, she's on a compounded CBD with a specific terpene blend. And she has a compounded CBN because she likes to have them separate so that she can modulate herself depending on what sort of day she's having.” Wren shares. “It’s impressive.”
This flexible, modular approach helps patients engage more actively with their treatment plans and reduces the risk of overmedication. It also allows clinicians to introduce new cannabinoids incrementally, observing individual responses without confounding effects.
The Impact of Extraction and Refinement
Cannabis extraction and refinement techniques have a profound effect on the delivery method therapeutic action of the final product. Crude extracts, typically produced via ethanol extraction and left minimally refined, tend to retain a broader spectrum of terpenes and minor cannabinoids, which may result in a more robust entourage effect.
Some patients report needing a smaller dose of minimally processed oils to achieve therapeutic effects compared to highly refined distillates.
Conversely, products that undergo multiple refinement steps (such as rotary evaporation or short-path distillation) may increase the purity and potency of individual actives like THC or CBD but at the cost of degrading or eliminating the delicate terpenes. Patients experience this when trying to find the right formula for their symptoms, formulators and prescribers know well that two 10:10 products can differ drastically in therapeutic effect, despite appearing identical in terms of THC:CBD ratio.
To compound the complexity for medical cannabis prescribers is a lack of transparency within the supply chain. As Dr Wren points out, suppliers may not even know the origin of a given batch, particularly in business-to-business (B2B) arrangements where extract sources can change without notice. Companies may not have to advise of changes in refinement protocols, making it difficult for clinicians to guarantee patients reliable products, leading to variability in therapeutic outcomes.
Clinical Courage in an Evolving Space
Scientifically, legislatively, and clinically, this is a fast-moving space. For prescribers, this evolution demands skills that are evident in Dr Joel Wren’s approach, a combination of data-driven pragmatism with compassionate flexibility.
As the market expands and novel technologies become more sophisticated, personalised care will remain the cornerstone of effective cannabinoid therapy.
If you're a prescriber, pharmacist, or healthcare professional navigating the complexities of cannabis prescribing in Australia, consider contributing your insights to the Insiders Extract. Contact our editorial team, we're always keen to include perspectives from practitioners, patients and industry experts.
Dr. Joel Wren is a General Practitioner and a pioneering medicinal cannabis clinician based in Adelaide, South Australia, with over 5 years of specialised experience in cannabinoid medicine. As an Authorised Prescriber and current Steering Committee Member of Cannabis Clinicians Australia (formerly president of the Australian Chapter of the Society of Cannabis Clinicians), Dr. Wren has been instrumental in advancing medicinal cannabis access and education in Australia. He holds Fellowship with the Royal Australian College of General Practitioners (FRACGP) and is Board Certified in Lifestyle Medicine, with particular expertise in palliative care and mental health. Dr. Wren's holistic approach to medicine encompasses social, mental, physical, and nutritional health aspects, and he has represented Australian cannabis clinicians on the international stage, including presenting to the United Nations Commission on Narcotic Drugs regarding medicinal cannabis rescheduling.
Disclaimer: This information is shared with a global readership for educational purposes only and does not constitute medical or business advice. All patient-related information has been de-identified OR fictional to protect privacy. Nothing in this article is intended to promote the use or supply of medical cannabis to members of the public.