Are Cannabinoids With Cancer Immunotherapy Causing Early Death? – A Call For Caution And Further Study
Article Written by Dr Ben Jansen
Read time: 5-7 mins
In recent years, cannabis has increasingly been integrated into medical treatments, including cancer care, for its potential benefits in symptom management. However, concerns are emerging regarding cannabis's interaction with cancer immunotherapy, specifically its impact on treatment response rates.
As both a physician involved in the medicinal cannabis industry and an advocate for patient care, I find the discussion and patient informed consent around this interaction critical. Two key studies on this topic offer preliminary data suggesting that cannabis may reduce immunotherapy efficacy, yet the results are limited and controversial, warranting caution and additional research.
Study Overviews and Findings
The first study by Taha et al. (2019) examined the immunotherapy radiological response rate (RR), progression-free survival (PFS) or overall survival (OS) in patients receiving nivolumab, an anti-PD-1 immunotherapy, for advanced cancer, including lung cancer, renal cell carcinoma, and melanoma. This retrospective analysis compared two groups: those on nivolumab alone (89 patients) and those on nivolumab with concurrent cannabis use (51 patients).
Findings showed a notably lower RR in patients using cannabis (15.9%) than in those on nivolumab alone (37.5%), with a statistically significant odds ratio of 3.13. The response rate was measured using radiological evaluation of tumours, and analysis excluded patients with advanced disease with survival of less than 2 months. This suggests that patients using cannabis had approximately three times the likelihood of poor immunotherapy treatment response. Notably, cannabis use did not significantly impact PFS or OS.
The second study by Bar-Sela et al. (2020), which was prospective, aimed to validate and expand on Taha’s findings with a separate cohort of patients. This study compared 34 patients receiving immunotherapy and using cannabis versus 68 patients receiving immunotherapy but not using cannabis. All patients were receiving immunotherapy as either first- or second-line treatment. The cannabis patients were mostly using inhaled cannabis.
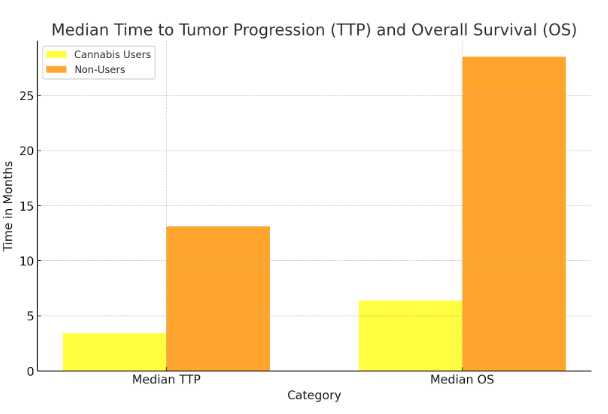
The study reported showing that the median time to tumour progression on radiological imaging for cannabis users was only 3.4 months versus 13.1 months for non-users (95% CI, 1.8–6.0 vs 95% CI, 6.0-NA). Furthermore, the study also reported the median overall survival for cannabis users was 6.4 months vs a much longer 28.5 months for nonusers, with significant log-rank tests p = 0.0025 and p = 0.0009, respectively (95% CI, 3.2–9.7 vs 95% CI, 15.6-NA). This study, however, faced critique for data accuracy and methodological transparency, as did the Taha study.
Comparative Analysis and Interpretation
Concerns raised by Piper et al. (2024) in the medical journal Cancers identified inconsistencies in data reporting and statistical discrepancies, undermining confidence in both of the study's findings. Re-analyses questioned whether baseline demographic differences between groups could account for the observed outcomes.
The Piper team reported identifying statistically significant differences for the Taha study; in cannabis users vs users for age (62yrs vs 67.7yrs), smoking status (56.9% vs 40%), liver metastasis (65% vs 19%), and immunotherapy as a second line therapy (85% vs 55%). The Piper team also commented on the Bar-Sela study “Of 22 statistics in the prospective report, four could not be repeated using the same statistics”, multiple misreporting or errors in analysis, and significant differences in cohort demographics.
Despite both studies suggesting a possible negative interaction between cannabis and immunotherapy, their methodologies and findings have invited scrutiny. Factors such as smoking and other lifestyle elements, which heavily influence cancer risk and treatment outcomes, should be carefully considered when assessing cannabis’s role in immunotherapy efficacy, cancer progression and when interpreting the studies. Piper et al. do not dismiss a possible negative interaction between cannabis and immunotherapy but point towards these as possible confounding factors in both of these preliminary studies.
One of the challenges in interpreting these studies is the inherent complexity of cannabis as a therapeutic agent. Cannabis affects the immune system through its active compounds, THC, CBD and the minor cannabinoids, which are known to modulate immune cell functions, and in some in vitro and in vivo studies to inhibit cancer cell proliferation and metastasis, while also promoting apoptosis and suppressing cancer-related angiogenesis (4). This immune modulation may theoretically counteract immunotherapy, but definitive conclusions are premature given these studies’ limitations, such as the sample sizes, the infancy of the research and potential demographic imbalances.
Caution in Clinical Practice
These findings hold particular relevance for patients considering or currently using medicinal cannabis during immunotherapy. As medical practitioners, we must weigh the benefits of cannabis in managing cancer-related symptoms (such as pain, nausea, and anorexia) against its potential to compromise treatment efficacy. While cannabis has a promising role in supportive cancer care, these early findings advocate for careful consideration when patients are concurrently undergoing immunotherapy.
As someone engaged in the medicinal cannabis industry, it is crucial to approach the results Taha and Bar-Sela studies with an open mind. The therapeutic potential of cannabis in oncology is still developing, and its integration with immunotherapy may carry unintended risks. Therefore, clinicians are advised to exercise caution - ensuring patients are well-informed of potential interactions is essential until further research provides clearer guidance.
My experience with Australian oncology patients using medicinal cannabis is that the majority will use oral medication rather than inhaled cannabis, where inhaled cannabis was predominant in the Taha and Bar-Sela studies. A further consideration for patients is the link between smoking tobacco and metastatic disease progression and cancer survival.
Future Directions and Need for Rigorous Research
The discrepancies in these studies highlight a need for rigorous, well-designed prospective trials. Future studies should aim to control for variables such as cancer type, cannabis dosage, and patient lifestyle factors, Particularly tobacco use, which may confound results.
Data transparency is vital to facilitate independent verification and bolster public and scientific trust in the findings. Additionally, larger studies should be commissioned to improve statistical power, and considering the Australian Government currently funds immunotherapy, regulatory bodies such as the TGA should require pharmaceutical companies to make their findings publicly available.
While cannabis holds promise as an adjunct to cancer care, particularly in symptom management, these studies underscore the importance of balancing innovation with prudence. As the field of immunotherapy advances, so too should our understanding of how adjunctive therapies, like cannabis, may influence patient outcomes. With further research, we hope to provide cancer patients with safe and effective treatment pathways that optimise their care and quality of life.
Taha, T., Meiri, D., Talhamy, S., Wollner, M., Peer, A., & Bar-Sela, G. (2019). Cannabis Impacts Tumor Response Rate to Nivolumab in Patients with Advanced Malignancies. The Oncologist, 24(4), 549-554. doi:10.1634/theoncologist.2018-0383
Bar-Sela, G., Cohen, I., Campisi-Pinto, S., Lewitus, G.M., Oz-Ari, L., Jehassi, A., Peer, A., Turgeman, I., Vernicova, O., Berman, P., Wollner, M., Moskovitz, M., & Meiri, D. (2020). Cannabis Consumption Used by Cancer Patients during Immunotherapy Correlates with Poor Clinical Outcome. Cancers, 12(9), 2447. doi:10.3390/cancers12092447
Piper, B.J., Tian, M., Saini, P., Higazy, A., Graham, J., Carbe, C.J., & Bordonaro, M. (2024). Immunotherapy and Cannabis: A Harmful Drug Interaction or Reefer Madness? Cancers (Basel), 16(7), 1245. doi:10.3390/cancers16071245. PMID: 38610922; PMCID: PMC11011043.
National Academies of Sciences, Engineering, and Medicine; Health and Medicine Division; Board on Population Health and Public Health Practice; Committee on the Health Effects of Marijuana: An Evidence Review and Research Agenda. The Health Effects of Cannabis and Cannabinoids: The Current State of Evidence and Recommendations for Research. Washington (DC): National Academies Press (US); 2017 Jan 12. Available from: https://www.ncbi.nlm.nih.gov/books/NBK423845/ doi: 10.17226/24625
Dr Ben Jansen is a founder of Cannabis Doctors Australia, CDA Clinics and Canview, and a current Executive Director for Australian Health and Queensland Hemp. Dr Jansen has family financial interests in Vitura Health Limited and other medicinal cannabis companies. Dr Ben Jansen is a contracting Senior Medical Advisor for Vitura Health Limited. No funding was received to produce this article.
Disclaimer: This information is shared with a global readership for educational purposes only and does not constitute medical or business advice. All patient-related information has been de-identified OR fictional to protect privacy. Nothing in this article is intended to promote the use or supply of medical cannabis to members of the public.